CARRE will address the specific medical domain of cardiorenal disease and comorbidities as this is a very common, life threatening and costly condition and because it also presents a number of challenges and opportunities for the demonstration of CARRE outcomes.
Cardiorenal syndrome (CRS) is the condition characterised by simultaneous kidney and heart failure while the primarily failing organ may be either the heart or the kidney. Very often the dysfunction occurs when the failing organ precipitates the failure of the other. The cardiorenal patient (or the person at risk of this condition) presents an interesting case example for addressing and demonstrating novel patient empowerment services for personalized disease & comorbidities management and prevention for a number of reasons:
- chronic cardiorenal disease has an increasing incidence and a number of serious (and of increasing incidence) comorbidities, including diabetes and hypertension, and may lead to serious chronic conditions such as nephrogenic anemia, renal osteodystrophy, peripheral neuropathy, malnutrition, as well as cardiovascular disease, and eventually death; patients usually present other comorbidities, such as diabetes complications (blindness, neuropathy, severe atherosclerosis, amputation), various systemic disease (e.g. rheumatoid arthritis, lupus erythematosus), malnutrition, respiratory and liver failure, age-related disease (e.g. Parkinson, Alzheimer), tumour, stroke, etc.
- prevention plays an important role for the various stages of cardiorenal disease evolution, from normal health condition, to chronic disease, to end-stage renal deficiency and/or heart failure;
- life style, diet and adherence to therapy are of major importance;
- cardiorenal disease represents and covers both chronic illness as well as acute episodes;
- requires self-management and personal monitoring;
- the patient is treated in a variety of places: at home, in primary care, in the outpatient clinic, in the clinic, in surgery (fistulas, grafts, etc.), even in the intensive care unit;
- the patient generally may lead a normal life, and may move, even across countries (for professional and recreational reasons);
- a number of alternative treatments and interventions are available (especially for end stage renal disease); and
- a number of alternative providers for treatment are also available.
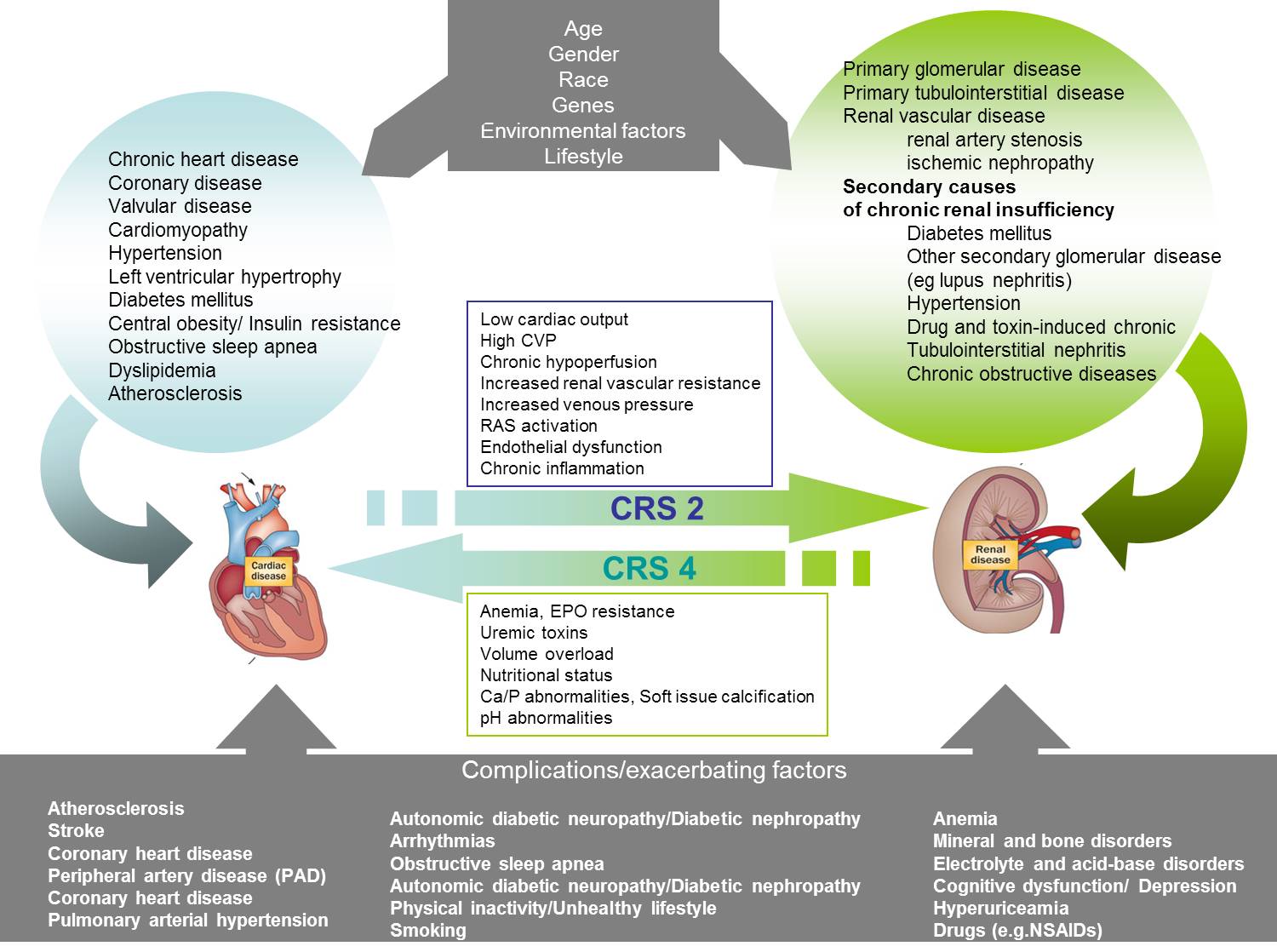
There is no single definition that appropriately describes CRS. Prof. Claudio Ronco of San Bortolo Hospital, Vicenza, Italy defined recently the cardiorenal syndrome as a pathophysiologic disorder of the heart and kidneys whereby, acute dysfunction of one organ may induce acute or chronic dysfunction of the other. Such interactions represent the pathophysiological basis for a clinical entity called cardiorenal syndrome. Current medical research identifies 5 different types of the cardiorenal syndrome.
Cardiorenal syndrome Type 1 (acute CRS) reflects an abrupt worsening of cardiac function (acute heart failure) leading to acute kidney injury (AKI). Acute kidney injury is commonly defined as an abrupt decline in renal function, over the course of hours to weeks.
Cardiorenal syndrome Type 2 (chronic CRS) comprises chronic abnormalities in cardiac function (e.g. congestive chronic heart failure) causing progressive chronic kidney disease.
Cardiorenal syndrome Type 3 (acute renocardiac syndrome) is characterized by an abrupt and primary worsening of renal function leading to acute cardiac dysfunction.
Cardiorenal syndrome Type 4 (chronic renocardiac syndrome) describes a state of chronic kidney disease contributing to decreased cardiac function, left ventricular hypertrophy, cardiac hypertrophy, diastolic dysfunction and/or increased risk of adverse cardiovascular events.
Cardiorenal syndrome Type 5 (secondary CRS) reflects a systemic condition causing both cardiac and renal dysfunction. Sepsis, diabetes mellitus, systemic lupus erythematosus are examples of such diseases affecting both renal and cardiac function. The systematic information on type 5 CRS is limited, although there is an appreciation that as many organs fail in this setting, mortality increases.
CRS Type 1 and CRS Type 3 include acute conditions (acute heart failure and acute renal failure) which need an urgent management. These patients should be admitted to hospital and treated under the supervision of specialists. CARRE Project concentrates on chronic states and outpatient services, thus mainly considers CRS Types 2, 4 and 5.
Considering the complex and bi-directional relationship between the heart and the kidneys, a subdivision of CRS into 5 different subtypes seems to provide a more concise and logically correct approach. The depth of knowledge and complexity of care necessary to offer best therapy to these patients demand a multidisciplinary approach, combining the expertise of cardiology, nephrology and critical care.
In general, cardiorenal syndrome is a complex condition, with a large number of factors and conditions related to it. Cardiac and renal axes interfere through risk factors, comorbidities, and complications. The pathogenetic interaction is demonstrated in the figure. One can distinguish an initial phase where the person is not yet formally diagnosed with a disease. Then, there are patients that have either heart or kidney disease. In this stage, there is an increased risk of one failing organ to lead to failure of the other, and thus lead to cardiorenal syndrome. Finally, patients with either one failing organ or with cardiorenal syndrome have an increased risk for entering end stage renal disease where renal function must be substituted with dialysis), and/or end stage heart failure. Such patients present also an increased risk for developing a number of other complications (as shown in the bottom of the figure).
CARRE takes into account all stages described above. An overview of current medical evidence on major conditions and comorbidities related to the project is given in Deliverable D.2.1. Domain Analysis and Use Cases, available for download from the project website (www.carre-project.eu).
Author: Stefanos Roumeliotis, Dimitris Papazoglou, DUTH
Date: 5 March 2014