The concept of patient empowerment has emerged as a new paradigm that can help improve medical outcomes while lowering costs of treatment by facilitating self-directed behavior change. Patient empowerment has gained even more popularity since the 1990’s, due to the emergent of eHealth and its focus on putting the patient in the centre of the interest. Current literature provides systematic reviews of the area, and shows that well defined areas (or dimensions) have eventually emerged in the field. We argue that patient empowerment also should be treated as a cognitive process. This will be used to design the appropriate methodology and tools for a systematic evaluation of CARRE intervention and its outcomes.
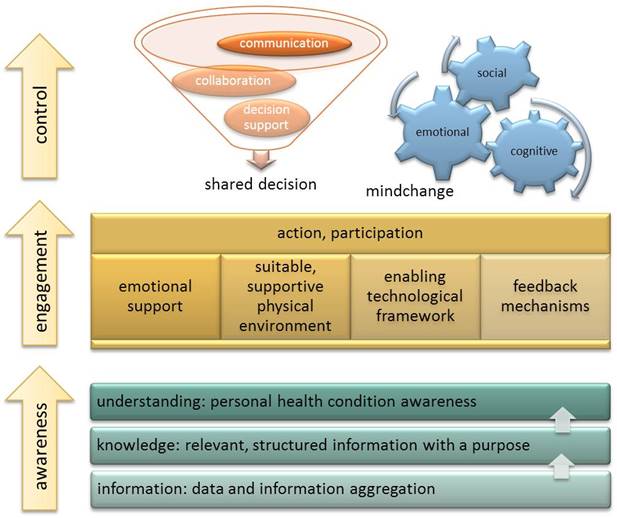
In particular, following the overall approach of cognitive psychology, we propose to treat patient empowerment in terms of three levels of increasing complexity and importance: awareness, engagement and control.
The first and most basic level refers to the complex task of health awareness. The patient (or the healthy citizen in general) should be aware of: his or her own health status; health related risks and lifestyle or environment induced hazards;potential disease progression to more severe stages; potential disease transition to other comorbidities; measures needed to stay healthy and/or prevent disease occurrence, progression or transition. This level corresponds to the educational dimension as in current literature. However, we believe that it is more appropriate to treat it as a personal awareness of one’s own health rather than the process of formal education. This underscores the fact that the patient should clearly understand the implications of the information provided and is able to act upon it.
Participation, the second level of patient empowerment, strives to achieve patient engagement in the health care process. Here we should emphasize active and proactive participation in managing the disease and its treatment and in preventing disease progression and transition. Successful patient participation can really be achieved only when the patient is health aware. However, this is not the only prerequisite. The patient additionally needs emotional strength, a suitable, supportive physical environment, an enabling framework and last but not least accurate feedback in order to be able to re-adjust participation. Emotional strength can generally be reinforced by easing the communication with health providers and most importantly within social groups. Both can be easily supported by common eHealth interventions that allow an easy and seamless communication with health providers or provide the environment for on-line social support groups. Creating a supportive physical environment may prove more intriguing. As we cannot easily alter physical environments to help patients, we could instead try to alter something equally important: the perceived environment. Here, future eHealth interventions should provide the means to identify resources and opportunities the environment already provides, which the patient (or its digital assistant) can exploit to increase the level and quality of participation in disease management.
Control in this context can include two different aspects: decision making and mind changing. Decision making refers to a collaborative process where patient and health professionals discuss and interact to reach a shared decision. A prerequisite for this is the patient to be health aware and also actively involved in her health management. Only then, the patients’ participation in decision making should be effective. However, this aspect of control involves extensive communication and collaboration. Both are widely supported by current eHealth applications in a variety of ways, including also advanced collaboration environments and shared digital spaces. Some interesting examples include the emergent technology of personal health records, owned by the patients themselves, who however can give targeted access to their health providers when needed. Also considerable research work is available in the field of medical decision support systems, which can be generally viewed as either (a) the so-called ‘strong’ artificial intelligence systems whose behaviour is at some level indistinguishable from humans; or (b) an alternative approach that looks at human cognition and decides how it can be supported in complex or difficult situations, something like a form of ‘cognitive prosthesis’ that will support the human in a task.
This novel empowerment model has been published as a funded CARRE intermediate result: E. Kaldoudi, N. Makris, Patient empowerment as a cognitive process, Proceedings of HealthInf2015: the 8th International Conference on Health Informatics, BIOSTEC 2015, Lisbon, Portugal, January 12-15, 2015 .
Authors: Eleni Kaldoudi, Nikos Makris (DUTH)
Date: 29 October 2014